Hearing loss is one of the most common health conditions affecting older adults, but it affects individuals of all ages, from newborns on up. Known for its negative impact on communication, age-related hearing loss, if left untreated, can lead to depression and other health problems as well. Despite the prevalence of hearing loss among older adults, a number of access barriers has contributed to the low uptake of hearing healthcare services.
The Arizona Telemedicine Program Blog, Category: mHealth
There’s a lot of buzz in every industry around the Baby Boomer population these days. After all, this remarkably large group of adults is the biggest in history to face the issues of retirement and aging. That means aging Baby Boomers will bring challenges to our healthcare system over the next few years.
One of the biggest issues at hand is the increasing shortage of healthcare professionals to meet this aging population’s needs. There is hope on the horizon, however.
The Association of American Medical Colleges reported in May the results of its 2017 Medical School Enrollment Survey, which found that medical school enrollment has increased 29 percent since 2002-2003.
Telemedicine is growing with a forecasted market increase of 16.8 percent from 2017 to 2023. It is already used by more than 50 percent of hospitals in the United States and close to 1 million Americans, thanks to its cost efficiencies and easy access to healthcare services.
While there are many benefits to telemedicine, they don't all come without valid concerns. The great news is that you can overcome these concerns by having a plan. Here are seven telemedicine concerns to take into account and effective strategies for overcoming them.
Telemedicine might sound like a strange fit for an industry that depends on human touch. For most of us, it's hard to imagine seeking treatment from a doctor using a screen or digital portal, rather than face-to-face in an office. But it’s been catching on for several years in many fields, including long-term care.
That’s because telemedicine provides solutions for several longstanding problems, including accessibility to care; the limited mobility of some patient communities including the disabled and the elderly; and a generally inadequate patient-to-doctor ratio in many areas.
Telemedicine might redefine long-term care as we know it. But first, we have to remove some of the uncertainty and even a bit of a stigma around the technology.
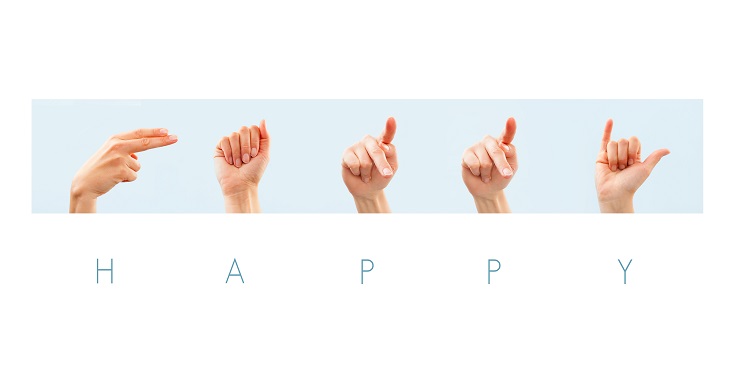
Note: This article adheres to the common use of two terms used to identify people who are Deaf or have hearing loss. The term Deaf (with a capital D) is used to describe individuals who do not hear and are “cultural” sign language users, while the term deaf (with a lower-case d) describes people who may lip-read and/or use hearing aids.
The expansion of telehealth services across the country has made it possible for almost anyone with a non-emergency medical problem to access a doctor by smart phone, pad or laptop, often within minutes, or at least, the same day. But for the Deaf and hard of hearing, access to telehealth providers such as Teladoc, American Well and others is more of a challenge.
The reason is simple: a videoconferencing session requires participants to hear what the person on the other side of the screen is saying.