The 2026 policy landscape signals a shift toward "tele-permanence" with the bipartisan FY26 funding package extending Medicare telehealth flexibilities through 2027 and the Hospital-at-Home program through 2030. Key updates include the permanent status of most telehealth codes and more flexible Remote Therapeutic Monitoring (RTM) options, such as new device supply codes for shorter 2–15 day collection periods and a 10–19 minute treatment management code. With FQHC/RHC billing via G2025 extended through 2026 and expanded support for behavioral health, CMS is establishing virtual care as a cornerstone of high-quality rehabilitation.
The Arizona Telemedicine Program Blog, Category: Providers
We had the opportunity to speak with Dr. Amit Algotar, MD, PhD, MPH, FOMA, FACPM who leads a telehealth-based lifestyle weight loss clinic at Banner University Medical Center South. His innovative approach focuses on using lifestyle modifications as a primary treatment modality for managing and preventing chronic conditions like cardiovascular disease, diabetes, and even certain cancers. In this Q&A, Dr. Algotar shares the philosophy behind his work, the impact he’s seeing, and how telehealth is helping him reach more patients.
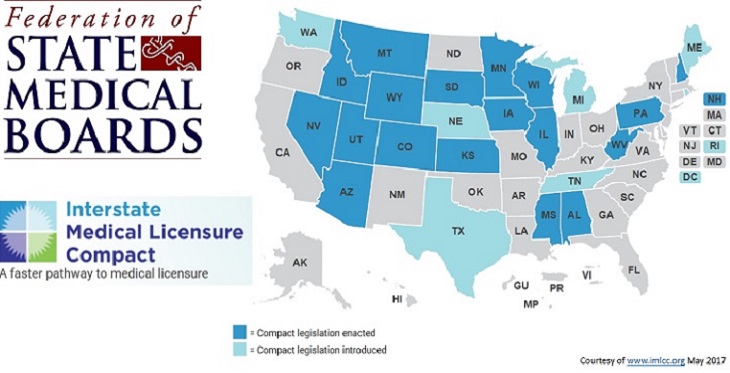
In a watershed moment for the expansion of telemedicine, the Interstate Medical Licensure Compact Commission is now processing applications to allow physicians to practice telemedicine across state lines with greater ease. Nineteen states have passed legislation to adopt the Interstate Medical Licensure Compact, which allows physicians to obtain a license to practice medicine in any Compact state through a simplified application process. Under the new system, participating state medical boards retain their licensing and disciplinary authority, but agree to share information essential to licensing, creating a streamlined process.
The European Psychiatric International Congress, held in Madrid last month, drew behavioral health professionals from around the world, including Herbert Schwager, PhD, a clinical psychologist from the town of Willow, Alaska.
Dr. Schwager was invited to the prestigious gathering to present his paper on “The 21st Century House Call.” The paper summarized his research comparing the efficacy and patient satisfaction of face-to-face psychotherapy sessions with tele-behavioral medicine sessions, with patient and therapist meeting via secure video conference sofrware.
Dr. Schwager’s study involved 400 patients. Two hundred were followed via tele-behavioral medicine, and the other 200 in face-to-face meetings. Patients were studied over a two-year period.