Congratulations to The Arizona Republic on its 125 years of publishing in Arizona. As part of its anniversary celebration, the newspaper compiled several historical Top 10 lists, including “Top 10 Health Stories from Arizona in the past 125 years,” by Ken Alltucker.
The list includes the 1918 flu pandemic, Arizona’s Medicaid launch, the state’s first heart-transplant surgery, formation of an early multi-hospital system (Samaritan Health, now Banner Health), hosting of a tuberculosis colony in the 1920s and 30s, producing and testing scorpion anti-venom, pioneering brain surgery, making strides in genomic medicine research, the Affordable Care Act, and telemedicine advances.
Ronald S. Weinstein, MD, founding director of the Arizona Telemedicine Program (ATP), is pleased—but not surprised—that “Telemedicine Advances” made the Top 10 list. Arizona has been a national leader in telemedicine, starting with the establishment of the ATP at the University of Arizona in 1996 at the urging of then-Representative Robert “Bob” Burns, whom Dr. Weinstein refers to as “an amazing public servant in our state.” Dr. Weinstein was personally involved, himself, with early multispecialty telemedicine cases at the Massachusetts General Hospital in Boston, in 1968, as a resident physician, and has been doing pioneering work in telemedicine ever since.
To name just a few Arizona telemedicine milestones…
Since 1998, the ATP has met quarterly with the Arizona Telemedicine Council on Capitol Hill in Phoenix to present telemedicine activities and advances throughout the state. There has always been a lot to report, including the ATP’s same-day mammogram results for Native American women in Tuba City; the more than 150,000 telepsychiatry sessions between doctors and rural patients via the Northern Arizona Regional Behavioral Health Authority network; teleconsultations from University of Arizona specialists to doctors and patients in Nogales, Yuma, and Sells; Carondelet Health Network’s telecardiology and telestroke consultations to southern Arizona rural hospitals; and the million-plus teleradiology cases throughout the state.
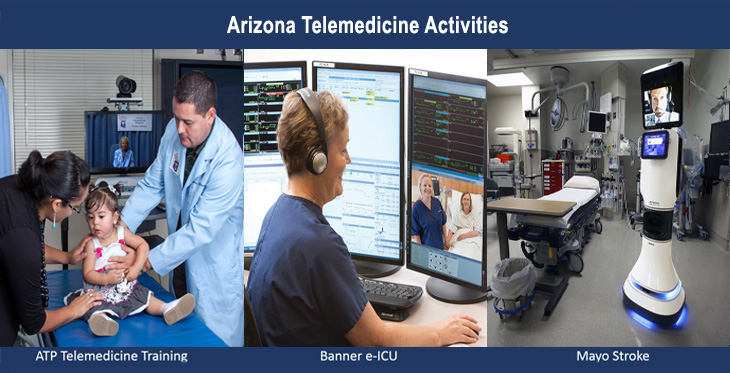
Today, Arizona remains a hotbed of telemedicine activity. Along with the ATP, the Republic article mentions the Mayo Clinic telestroke program, where neurologists connect to emergency room doctors in rural Arizona to evaluate patients with stroke symptoms, and the Banner Health eICU program, which links its multiple intensive care units to tele-intensivists at a single site in Mesa. Both programs are featured in the ATP’s Arizona Telemedicine Magazine, along with many other telemedicine success stories, including an Indian Health Service teleophthalmology program that screens for diabetic retinopathy, the leading cause of blindness in working-age adults; “Care Beyond Walls and Wires,” a Northern Arizona Healthcare initiative that monitors congestive heart failure patients and helps them avoid hospital readmissions; teleconsultations by the Arizona Burn Center to determine whether a patient needs to be transported or can be treated locally; the ATP’s ¡Vida! breast cancer support group and patient/provider tele-education program; and HIV/AIDs patient treatment throughout northern Arizona via the North Country Healthcare telemedicine program. Telemedicine programs in Arizona are growing by leaps and bounds, with many more successes and startups too numerous to list here.
Multiple medical specialty services such as those mentioned above are available to Arizona’s rural hospitals and other organizations via telemedicine technology. The ATP’s national Telemedicine & Telehealth Service Provider Directory lists 25 telemedicine service provider companies (10 of them based in Arizona) currently offering services such as telecardiology, teledermatology, telestroke, and telepsychiatry to hospitals, clinics, schools, and other organizations in Arizona—and more companies that plan to bring services to Arizona in the near future.
Telemedicine activities beyond medical services
Arizona is home to global leaders as well as startups in telemedicine technology, including GlobalMed, which made the Deloitte Top 100 fastest growing tech companies list in 2012, and T-MedRobotics, which makes a remote-controlled echography system for areas without local sonography experts.
Our state is a national telemedicine expertise leader as well. ATP staff and other Arizona telemedicine leaders have published a wealth of books, chapters, and papers over the past 20 years, and have presented at hundreds of state and national meetings. The ATP boasts a President Emeritus (Dr. Weinstein), for being a “pioneer in telemedicine,” and two past presidents (Elizabeth A. Krupinski, PhD, and Dr. Weinstein) of the American Telemedicine Association (ATA), along with several past and current chairs of ATA Special Interest Groups.
The ATP has been offering its Arizona Telemedicine Training Program—with two tracks, each offered three times per year—for 17 years. The training programs, offered simultaneously in ATP training facilities in Phoenix and Tucson, are linked by video conferencing, and are among the few telemedicine education courses accredited by the American Telemedicine Association. Dr. Weinstein notes that “many current, and future, telemedicine leaders have passed through our training program. At last count, over 1,000 individuals, from over a hundred organizations, have done their telemedicine training with us.” The ATP also houses the Southwest Telehealth Resource Center, a federally funded assistance center serving the southwestern states. And groups such as the Northern Arizona Telemedicine Alliance have formed to share information and collaborate on projects.
With all these burgeoning telemedicine programs, companies, education, services, meetings, and expertise in Arizona, it’s no surprise that telemedicine would make the Arizona Republic’s “Top 10 List of the Most Important Health Stories in the State over the Past 125 Years.” Telemedicine saves lives, reduces costs, and improves patient outcomes and satisfaction. Clearly, telemedicine has gone “main stage” in Arizona.
This article was co-authored by Nancy Rowe and Kristine Erps. Kris Erps serves as the associate director for administration Arizona Telemedicine Program and as the project administrator for Southwest Telehealth Resource Center. She is a member of the Arizona Rural Health Association and the ATA Special Interest Group Business and Finance and served on the HRSA Focus Group on EHR Adoption and Meaningful Use. She has been with the ATP since 2000.