A home run, or a “four-bagger” in entrepreneur-speak, in telemedicine or telehealth is: 1) a patient service which is equivalent to an in-person service in terms of effectiveness including patient and provider satisfaction; 2) is sustainable; 3) is cost effective; and 4) is a service that migrates into the mainstream of the US healthcare delivery system.
Telemedicine home runs have been a long time in coming.
A Hospital, An Airport, and Telemedicine
As I can personally attest, telemedicine actually got off to fantastic start at the Massachusetts General Hospital (MGH), in 1968. None of its services achieved four-bagger status back then.
Historically, the MGH linked to the Logan International Airport over a private microwave linkage. Services included teleradiology, telecardiology, teledermatology, telepsychiatry, and television microscopy (the predecessor to modern “telepathology” which I invented, patented, and commercialized years later). For roughly 8 years, a team of visionary MGH doctors delivered high quality telemedicine services, at a distance, to air travelers in transit, at a walk-in Logan Airport healthcare clinic 2.7 miles from MGH, as the crow flies.
Space Medicine On Earth
By the late 1960s, popular magazine’s featured articles describing remarkable MGH telemedicine success stories. Space medicine had caught the imaginations of millions of ordinary people. The general public could link MGH-telemedicine and space medicine, in the same breath. Telemedicine became earth-bound medicine’s counterpart to space medicine.
Of course, this was a human-interest bonanza for NASA. It made space medicine relevant to the average patient here on earth. NASA had won the billion-dollar bet on space medicine as a featured program for their first man-on-the moon landing enterprise back then.
Hooked: Television Microscopy Diagnoses
I was a MGH pathology resident from 1965-1970, and got caught up in the space race to the moon. I followed the progress of the MGH telemedicine program in Boston newspapers, and then, had the luck of the draw for a resident.
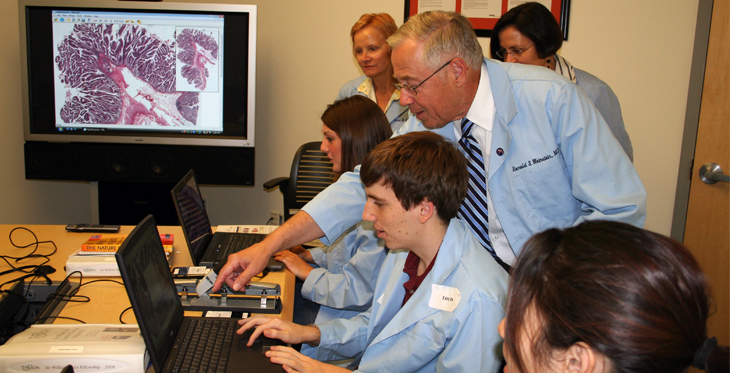
By chance, in April 1968, I was having lunch in the MGH cafeteria with MGH staff pathologist, Dr. Robert “Bob” Scully. We were on the surgical pathology service together. He was going to view some MGH-Logan Airport “television” microscopy cases right after lunch. Bob took me along and we signed out a few cases together. We also became life-long friends.
Thus, by chance, I got to help diagnose some of the first “television” microscopy glass slide video images coming in to the MGH telemedicine suite, on the first floor of the MGH White Building, sent from the telemedicine-enabled MGH-Logan International Airport clinic.
I still remember it vividly, as a transformative experience. I was immediately hooked on telemedicine. Years later, I realized that I had become an “accidental-outlier” for telemedicine, in the parlance of Malcolm Galdwell, in his description of the secrets for success for pioneers in innovations.
The First Telemedicine Service Home Run
Back to the MGH in the late 1960s and early 1970s. The first telemedicine service home run was teleradiology, a component of the MGH-Logan Airport telemedicine program.
Teleradiology had been deployed in Canada, around 1959, and then adopted by the MGH program in 1968.
Home run status was achieved decades later.
Today, teleradiology is quite ubiquitous, sustainable, cost effective, and is regarded by many to be mainstream medicine. Thus, a home run!
Teleradiology has been commercialized by dozens of companies. It’s heavily marketed and is benefitting millions of patients, every year. A home run and a done deal! But, not universally loved by hospital-based radiologists.
Next In Line for a “Four-Bagger”
Telestroke programs are in the line-up for the next home run. Telestroke is still a work in progress, but it may emerge as a cornerstone for the telemedicine field.
What makes telestroke a “must have” service is that it is undeniably cost effective, prevents permanent injury to the brain or even death, and the logistics are manageable by call centers.
World-class healthcare organizations, such as the Mayo Clinic, are stepping up into the lead as regional, and potentially national, leaders in telestroke. There are reimbursement issues but the return on investment is potentially so high, society will figure out how to make it work.
Almost everyone loves a home run. Not everyone loves baseball!