I was vacationing in a tiny, remote mountain town on the east coast last summer when I became ill. It was a Sunday evening and the local urgent care center didn’t open until the next morning. I didn’t want to wait 15 hours for urgent care, and I didn’t want to be driven to the regional ER, where I might have to wait a long time to be seen—and might be exposed to something contagious while in the waiting room.
Luckily, I had recently heard about one of the companies that provides urgent care visits via telemedicine. So I took out my iPad, loaded the app, and called in.
I was able to choose from a list of doctors; I agreed to pay the fee (about what my urgent care copay would have been, and certainly less than an ER visit would have cost); I entered my credit card info; and within a few minutes I was talking to the doctor I chose—all from my bed! The doc called in a prescription to the pharmacy I selected and I was feeling fine very shortly.
A Visit to the ER vs. Telemedicine
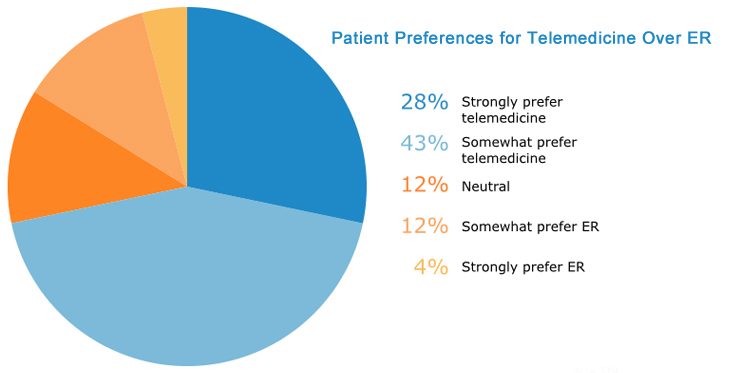
My experience jives with a recent survey conducted by medical technology reviewer Software AdviceTM, which found that only 16 percent of patients would prefer to seek care for a minor ailment at an emergency room if they also had access to telemedical services. The survey also found that, among patients who have not used a telemedicine service, 75% express interest in using one in lieu of an in-person medical visit.
Kathleen Irwin, a market research associate at Software Advice, says that, as of January 2015, patients spend an average of 133 minutes in the ER. Take that two-plus hours and add in the transport time to and from, and compare it to the approximately 10 minutes my virtual doctor visit took from start to finish.
Why Patients Choose Telemedicine
My experience is not unique: Patients in the survey who had used telemedicine, when asked to cite positive aspects of their most recent virtual appointment, cited “don’t have to travel” (21%), “comfort of home” (20%), “quick access to care” (11%), “shorter wait time” (10%), and “avoid waiting room” (8%) as among the top benefits. Interestingly, 21% also cited “high quality of care” as one of the benefits they experienced.
When I used the telemedicine service, I wasn’t expecting particularly high quality medical advice, but I knew what was wrong with me and what prescription was needed, so I didn’t mind experimenting. My experience was so positive, though, that I used the same vendor again—this time from home—in order to avoid a long trip to, and a wait at, my local primary care doctor’s office.
The care I received in both virtual visits (and I was able to choose the same doctor both times, even from two different states) was at least on a par with, if not superior to, the medical care I have experienced in recent urgent care visits.
The Insurance Hurdle
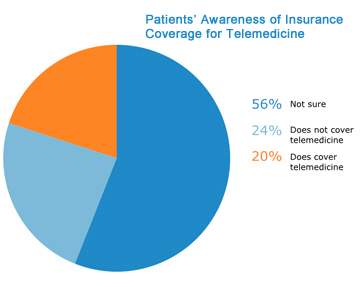 Market researcher Irwin says the average telemedical visit costs between $40 and $50. My visits were in that range and I consider the convenience and prompt service well worth the price. I assumed that my insurance wouldn’t pay for the visit, and, like me, more than half of the patients surveyed (56%) didn’t know if their health insurance covers visits conducted using telemedicine.
Market researcher Irwin says the average telemedical visit costs between $40 and $50. My visits were in that range and I consider the convenience and prompt service well worth the price. I assumed that my insurance wouldn’t pay for the visit, and, like me, more than half of the patients surveyed (56%) didn’t know if their health insurance covers visits conducted using telemedicine.
Arizona’s telemedicine parity law is “partial”—it covers only a few healthcare services and primary care, unfortunately, is not among them. We need to get telemedicine parity to the point where patients don’t have to wonder if they’re covered when they choose to see a doctor via telemedicine—because, according to the survey, studies suggest that the number of patients taking advantage of telemedicine will increase twentyfold over the five year period from 2013 (350,000 users) to 2018 (7 million users).
The Number One Concern
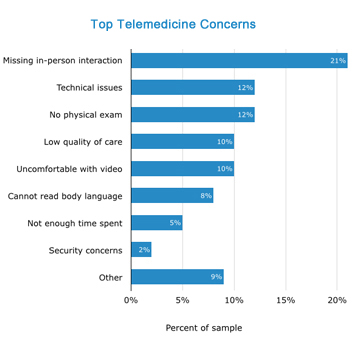 Patients in the survey also were asked to cite their top concerns about their most recent telemedicine visit. The number-one concern was “missing in-person interaction” (21%) with many pointing out that the visit was “colder” or “less personal” than an ordinary, in-person visit.
Patients in the survey also were asked to cite their top concerns about their most recent telemedicine visit. The number-one concern was “missing in-person interaction” (21%) with many pointing out that the visit was “colder” or “less personal” than an ordinary, in-person visit.
I personally didn’t feel that way, but that could be because I am very used to using videoconferencing to interact with others—and also, the provider I met with had a great “screen presence,” making me feel right at home.
Check out the full Patient Interest in Adopting Telemedicine survey to read more and see all the results.