Note: This article adheres to the common use of two terms used to identify people who are Deaf or have hearing loss. The term Deaf (with a capital D) is used to describe individuals who do not hear and are “cultural” sign language users, while the term deaf (with a lower-case d) describes people who may lip-read and/or use hearing aids.
The expansion of telehealth services across the country has made it possible for almost anyone with a non-emergency medical problem to access a doctor by smart phone, pad or laptop, often within minutes, or at least, the same day. But for the Deaf and hard of hearing, access to telehealth providers such as Teladoc, American Well and others is more of a challenge.
The reason is simple: a videoconferencing session requires participants to hear what the person on the other side of the screen is saying.
People who are Deaf or hard of hearing are seldom seen as people who have a disability. Unlike a blind person who walks with the support of a cane or a person who uses a wheelchair, people who cannot hear often use the term “invisible disability,” as theirs is not obvious to the public.
And yet, they comprise a significant portion of the U.S. population:
- A December 2016 report in JAMA Otolaryngology concluded that 18 percent of adults aged 20 to 69 have hearing loss in both ears, due to exposure to loud noise at work.
- The National Institute on Deafness and Other Communication Disorders reports that 25 percent of American adults aged 65 to 74, and 50 percent of those who are 75 or older, have disabling hearing loss.
- In Arizona, about 1.1 million people have a hearing loss, according to Emmett Hassen, licensing and certification coordinator for the Arizona Commission for the Deaf and the Hard of Hearing. And as many as 30,000 Arizonans were born Deaf, as Hassen was, and identify as "culturally Deaf."
“And about 20 percent of children have some form of hearing loss,” Hassen says. “In the old days there were boom boxes and you could really hear the sound from afar. “But today, with Bluetooth earphones and iPods, the in-ear headphones are close enough to the ear that they affect the eardrum more significantly. And that’s causing more hearing loss.”
In a recent webinar presentation, Hassen defined some of the various aids available to people with hearing loss. Licensed American Sign Language interpreters are commonly included in gatherings and public meetings, regardless of how many Deaf people are in attendance. Interpreters also may be available, for example, to Deaf patients in hospitals or nursing homes, arranged by their doctor or other healthcare provider, as required by law.
Timing can be an obstacle, however, as sign language interpreters usually have to be scheduled more than a week, or at least a day, in advance.
Video Remote Interpreting (VRI) is an alternative to videoconferencing, with interpreters connected through webcams, and is commonly used in hospitals around the country. Federal law requires hospitals to ensure VRI equipment displays high-quality video images, large enough to show the interpreter’s face, arms, hands and fingers; clear voice transmission; and trained hospital staff who can quickly and effectively set up and operate the VRI equipment.
Technology is advancing at such a rapid rate, some of what we consider breakthroughs today will be seen as old-fashioned before we know it.
But communication – for those who hear and those who are unable to hear clearly, or at all – is not all about high tech, Hassen reminds us.
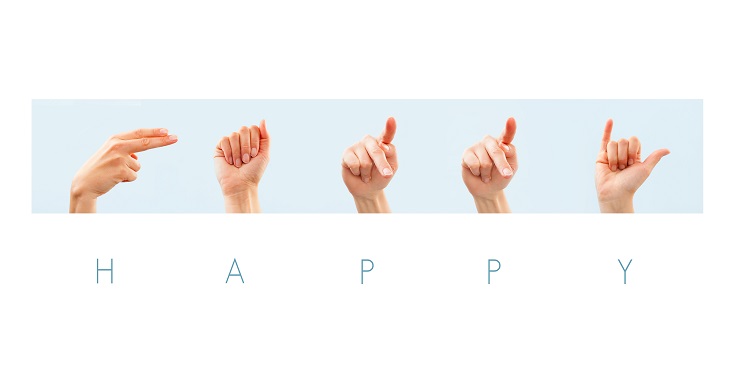
“Facial expressions are actually a part of American Sign Language,” he says. “In English we show emotion with our tone of voice. You can tell on the phone if someone is happy, sad or mad. And Deaf people have facial expressions, too. You can tell if we are happy, sad or mad. Facial expressions make a big difference.”