Although the education of medical and nursing students regarding telemedicine has lagged behind the implementation of telemedicine services, such as telestroke and telepsychiatry, that’s about to change.
A recent survey by the Association of American Medical Colleges documented a sharp increase in the number of medical schools offering telemedicine experiences to their students. Furthermore, medical schools are incorporating telemedicine training facilities in their state-of-the-art education buildings. The University of Arizona’s College of Medicine -- Tucson's new Health Sciences Innovation Building, scheduled to open in August, will include an “e-Classroom of the Future," designed by Ronald S. Weinstein, M.D., a pioneer in telemedicine and telepathology, a subspecialty of telemedicine. Dr. Weinstein is the founding director of the statewide Arizona Telemedicine Program, established by the Arizona Legislature in 1996, and headquartered at the University of Arizona College of Medicine --Tucson.
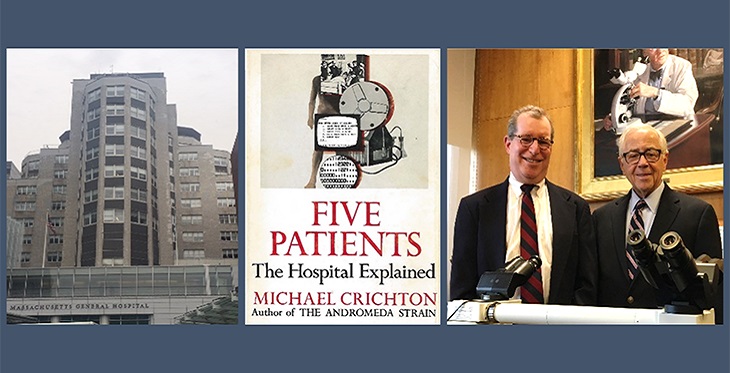
Historically, Dr. Weinstein diagnosed his first telemedicine cases as a third-year pathology resident at the Massachusetts General Hospital, in Boston, in April 1968, shortly after the start-up of the pioneering Logan Airport/Massachusetts General Hospital (MGH) telemedicine program.
Back in 1968, and for decades before, Logan collaborated with Massachusetts General Hospital to provide medical care for sick airline passengers and employees. An MGH doctor would drive to the airport and examine the patient at the airport’s walk-in clinic, then known as the Massachusetts General Hospital Medical Station. The clinic also was designed to help airport staff and physicians deal with emergency situations.
Dr. Weinstein, and Robert E. Scully, M.D., an MGH staff pathologist, rendered a diagnosis of “normocytic hypochromic anemia," by visualizing a blood smear on a glass slide, mounted on a “television” microscope located at the Logan Airport, 2.7 miles away from the MGH. This form of “television microscopy” was the forerunner to “dynamic robotic telepathology,” which Dr. Weinstein invented, patented, and successfully commercialized two decades later. According to the Oxford English Dictionary, Dr. Weinstein introduced the term “telepathology” into the English language.
In addition to Dr. Weinstein, two other Harvard Medical School (HMS) trainees, another MGH resident and a Harvard Medical School student, were recruited into this pioneering telemedicine service. One was Jay H. Sanders, MD, a senior medicine resident and colleague of Dr. Weinstein’s. Dr. Sanders went on to become a trusted telemedicine advisor for a number of countries, and a U.S. representative on high level international commissions. He also established a successful telemedicine consulting business. Michael Crichton, then a fourth year HMS student, did a two-week clinical rotation on the Logan Airport/MGH telemedicine service, in 1969. He described his telemedicine experiences, including a personal telemedicine patient encounter, in his book “Five Patients: The Hospital Explained.” The 26 year-old Crichton received his Harvard M.D. degree one month after “The Andromeda Strain,” his best-selling novel, was published. Weinstein remembers seeing the 6- foot, 9-inch tall Dr. Crichton wandering around the halls of the MGH, and seeing him in the MGH employee cafeteria eating lunch with the MGH Director, John H. Knowles, MD, who also played a significant role in Dr. Weinstein’s career.
The University of Arizona, and the State of Arizona, have benefitted from Weinstein’s highly visible roles as an inventor and innovator. Companies he co-founded have received "start-up-company-of-the-year” awards. The international award-winning T-Health Amphitheater, an “e-Classroom-of-the Future,” which Dr. Weinstein co-designed and developed over four years on the Phoenix Biomedical Campus, was dedicated by the University of Arizona’s President, Robert Shelton, PhD, in 2009, at a ceremony witnessed by a large audience packed with dignitaries. An array light microscope, which Weinstein co-invented with faculty members at the UA College of Optical Sciences, received international recognition as a leading-edge technology.
Prior to relocating to Arizona in 1990, Dr. Weinstein had established his reputation as an inventor and innovator, while chair of pathology at Rush-Presbyterian St. Luke's Medical Center and the Harriet Blair Borland Professor at Rush Medical College, in Chicago. In addition to inventing robotic telepathology, Dr. Weinstein organized the first public demonstration of the technology. In 1986, he used an SBS-3 satellite to transmit live robotic telepathology video images from a remotely-controlled robotic motorized light microscope at a U.S. Army base hospital, in El Paso, Texas, to a pathologist seated at a telepathology workstation of Dr. Weinstein’s design, situated in the impressive COMSAT corporation's board room, in downtown Washington, DC. The telepathologist rendered a diagnosis of “breast cancer” in a 66-year old woman, in front of 22 invited observers, including the Assistant Surgeon Generals’ of the U.S. Army and Air Force and academic leaders from the Washington area medical schools. The dramatic rendering of a diagnosis, via telepathology, for a woman 2,000 miles away, brought the observers to their feet for a round of applause. The demonstration, a glimpse into the future, was reported in the Washington Post, the International Wall Street Journal, and on NBC television.
In 1990, Dr. Weinstein, now well known as an innovator and successful entrepreneur, was recruited to the University of Arizona’s College of Medicine, in Tucson, Arizona, as its pathology chair. In Arizona, he established the first international telepathology service linking patients in China and Mexico to specialty telepathologists in the United States and created the award-winning Arizona Telemedicine Program, now in its 22nd year of operation.
With respect to the field of telemedicine, Dr. Weinstein says, “I constantly cheer telemedicine on. It’s my baby and I love my role in moving it forward. After all, being in a position to participate in the creation of a new field like telemedicine, to personally catalyze its diffusion around the world, and then to work on it as its cheerleader for the next half-century, brings a lot of perspective and satisfaction with it.
"Being in a position to continually create new things gives life an enduring purpose. That’s why we love innovation!”