Is telemedicine “as good” as a face-to-face patient visit? Take a few cues from television and movie professionals to make sure!
In today's digital world, we've all become visual image connoisseurs. Part of what we respond to is technical and part is artistic. It's largely the “artistic” portion in which meaning and emotion are created.
As such, telemedicine professionals would be wise to pay attention to certain artistic aspects, when creating the telemedicine patient/provider encounter.
Beyond the 'good enough' technical aspects of the telemedicine encounter – available bandwidth, relatively clear and fluid video, and audio of an acceptable level – there is a higher-quality bar that we, as telemedicine professionals, must strive to reach, in order to be trusted and to overcome objections that our viewers might have. Often, these objections may even be subconscious on the viewer's part, but still come into play, and nothing is harder to resolve than an unconscious objection!
Since long before I became involved in telemedicine, I was a television and video production professional, both in business and in private practice. I've also taught video production workshops for many years, including to adult learners. An important part of what I teach in these workshops is the “production values” that are essential to providing a high-quality viewer experience. These values are equally applicable to telemedicine and videoconferencing!
Fortunately, there are a few things that you can easily do, to achieve this objective. Among them are:
Image Composition, Lighting, Sound and Background Separation
Image Composition
There is a well-known technique for composing quality video images. It's known as the "rule-of thirds, as it specifies placing the subject's eyes one-third of the way down from the top of the screen. In telemedicine terms, doing so approaches a recommended 7-degree "angle of incidence" between the subject's eyes and the center of the camera lens. Angle of incidence creates an image in which patient and provider are looking directly at each other. When looking too high, or too low – the feeling of connection between patient and provider is lessened, and the patient's perception, rightly or wrongly, of “being heard.”
Another way to achieve this is to center the subjects on screen, eliminating unnecessary space above the subject's head. When framing two or more subjects, the same rule applies, on a sliding scale.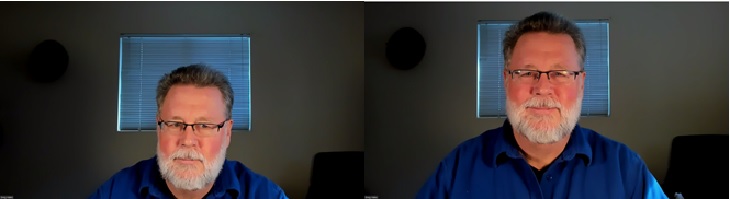
Lighting
Exam room lighting presents a real challenge for telemedicine. Though lighting may be sufficient in quantity, to avoid video artifacting (e.g. shimmery video), it is often of the wrong “color temperature," making it difficult for patient and provider skin tones to be accurately and realistically seen.
Usually, fluorescent lights are used in provider and exam rooms lighting is by fluorescent tubes, which makes patient skin tones look yellowish or greenish. Further, exam room lighting (usually from above, casts undesirable shadows on the subject's face, sometimes making them look angry or sad -- again, often unconsciously! Cameras and camera software provide color correction, called "white balance, which usually enables color correction.
It is possible that a busy teleprovider might miss a diagnosis, or misdiagnose a patient, based on inaccurate and/or unrealistic lighting, but "white balance" will usually correct the problem. The same lighting problem can be see from the patient's perspective, though appropriate teleprovider lighting may be easier to achieve.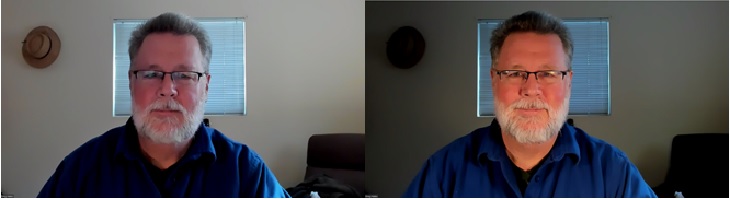
Lighting equipment recommendations can be found on the web.
Background
Perhaps nothing is more unprofessional looking than a cluttered wall or bookshelf behind the patient and/or teleprovider, but shared workspaces are prone to this. With a product called WebAround, the clutter can remain, but is no longer seen! Workspaces, especially shared workspaces, are prone to this. In the teleprovider's case, limiting/defining the provider's workspace will be a great help. One way to do this is using a product called the WebAround (www.webaround.com) – the same clutter as before, but no longer seen!

Sound
Very often, exam rooms have tile floors and not much furniture. This causes patient voices to echo, on the teleprovider's end – especially when the patient is at a distance from the micropohone. Distant patient plus hard ceilings can sometimes cause teleproviders to not be able to distinguish patients words – making the tele-encounter unnecessarily challenging. If it's not possible to add acoustical treatment to tele-exam room floors, moving the microphone as close to the patient as possible will help a great deal. Ideally, the microphone should be no more than 2 feet from the patient.

That's all for this time. Please feel free to email me with questions or comments and/or suggested topics for my next article. Happy telemed-ing!

